EyeKinetix®
Objectivity Meets Speed and Precision,
The Clear Choice for Pupillometry
Essential for comprehensive eye exams, EyeKinetix® accurately analyzes pupils for relative afferent pupillary defects, aligning with the AAO’s Preferred Practice Patterns® for glaucoma suspects and patients
NOW REIMBURSABLE WITH CPT CODE 95919

EyeKinetix® Objective
Binocular Pupillometer
Importantly, there is evidence that even subtle RAPDs may be clinically significant. EyeKinetix® makes it easy to accurately and objectively assess RAPDs and physiological anisocoria.

Clinical Applications
*Routine eye exams glaucoma suspects and patients
3rd cranial nerve palsies
Optic nerve, retinal or cerebral vascular disease, tumors, amblyopia
Multi-focal lens fittings
*Pupil testing is recommended by the AAO and AOA for POAG suspects and patients
EyeKinetix® is not cleared for the specific diagnosis of any condition.
Clinical Benefits
May aid in the detection of vision or even life-threatening disorders
Accurately measure and document physiological anisocoria
Objective: improve your confidence in routine and subtle RAPD assessment
Detailed, objectively quantified documentation of the presence or absence of an RAPD
Regulatory
FDA Listed | CPT Code 95919
Health Canada Licensed
A 21st century alternative to a 19th century test
Konan Medical has been dedicated to advancing objective binocular pupillary testing technology for ophthalmology and optometry for over a decade
The EyeKinetix® pupillometer utilizes high-definition video cameras under infrared conditions to record the bilateral pupil responses to monocular visual stimuli.
Unlike human observers that only see one pupil reflex at a time, EyeKinetix® simultaneously records both direct and consensual pupillary light reflexes.
Easy, objective, quantitative, delegated, reimbursable; an order of magnitude more detailed than the finest human observer.

Relative Afferent Pupillary Defect (APD/RAPD)
The APD is a measure of asymmetry which may occur with optic nerve, retinal, or cerebral vascular disease, and amblyopia, specifically when the disease or disorder is presenting asymmetrically. Pupil testing is a required part of a comprehensive eye examination, historically performed as a subjective observation (SFM), and considered by many clinicians as difficult to perform well.
Examples of disorders that may cause an APD:
- Glaucoma
- Amblyopia
- Optic neuritis / MS
- Optic nerve tumor
- Optic nerve infections or inflammation
- 3rd cranial nerve palsies
- Retinal detachment
- Intraocular tumor
- Retinal infection
- Alzheimer’s
- Autism
- Brain tumors
- Parkinson’s
- Traumatic optic neuropathy
Visibility of Pupils Through Grey Absorptive Lenses
Note that an APD of 0.3 light log units, which is considered subtle, means the affected eye ‘sees’ 50% less light than the unaffected eye.

The RAPDx® Test
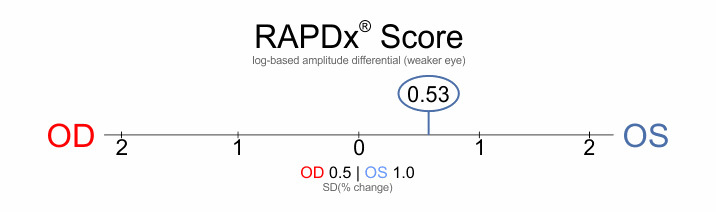
The RAPDx® score illustrated here indicates that the left eye sees less light (i.e. has the weaker response) and the averaged score is recorded as 0.53 (constriction amplitude differential) in this example.
Assessed independently as being comparable to the swinging flashlight method when quantified using neutral density filters.
NOTE: Pharmaceutical agents including prescribed, OTC, recreational drugs and abused substances, as expected, may affect pupil reflexes and their measures.
Scotopic-Photopic Pupil Measurements + IPD
Pupil dimensions, inclusive of asymmetry of pupil sizes can be helpful for functional pupil assessment, as well helping provide better understanding the contributions of optic zone dimensions in refractive surgery and complex multifocal IOl and contact lens selection.
Scientific and Clinical Publications
Effects of Age and Sex on Values Obtained by RAPDx® Pupillometer, and Determined the Standard Values for Detecting Relative Afferent Pupillary Defect
Satou, Tsukasa, et al. "Effects of age and sex on values obtained by RAPDx® pupillometer, and determined the standard values for detecting relative afferent pupillary defect." Translational Vision Science & Technology 5.2 (2016): 18-18.
Correlation Between Inter-Eye Difference in Average Retinal Nerve Fiber Layer Thickness and Afferent Pupillary Response as Measured by an Automated Pupillometer in Glaucoma
Sarezky, Daniel, et al. "Correlation between inter-eye difference in average retinal nerve fiber layer thickness and afferent pupillary response as measured by an automated pupillometer in glaucoma." Journal of Glaucoma 25.3 (2016): 312-316.
Correlation Between Intereye Difference in Visual Field Mean Deviation Values and Relative Afferent Pupillary Response as Measured by an Automated Pupillometer in Subjects with Glaucoma
Sarezky, Daniel, et al. "Correlation between intereye difference in visual field mean deviation values and relative afferent pupillary response as measured by an automated pupillometer in subjects with glaucoma." Journal of Glaucoma 23.7 (2014): 419-423.
Pupil-based detection of asymmetric glaucomatous damage – comparison of the Konan RAPDx® pupillograph, swinging flashlight method, and magnifier-assisted swinging flashlight method
Ali, Mohsin, et al. "Pupil-based detection of asymmetric glaucomatous damage-comparison of the Konan RAPDx® pupillograph, swinging flashlight method, and magnifier-assisted swinging flashlight method." Investigative Ophthalmology & Visual Science 54.15 (2013): 4811-4811.
Symmetry of the pupillary light reflex and its relationship to retinal nerve fiber layer thickness and visual field defect
Chang, Dolly S., et al. "Symmetry of the pupillary light reflex and its relationship to retinal nerve fiber layer thickness and visual field defect." Investigative ophthalmology & visual science 54.8 (2013): 5596-5601.
Accuracy of pupil assessment for the detection of glaucoma: a systematic review and meta-analysis
Chang, Dolly S., et al. "Accuracy of pupil assessment for the detection of glaucoma: a systematic review and meta-analysis." Ophthalmology 120.11 (2013): 2217-2225.
A novel computerized portable pupillometer detects and quantifies relative afferent pupillary defects
Cohen, Liza M., et al. "A novel computerized portable pupillometer detects and quantifies relative afferent pupillary defects." Current eye research 40.11 (2015): 1120-1127.
Estimation of Retinal Ganglion Cell Loss in Glaucomatous Eyes With a Relative Afferent Pupillary Defect
Tatham, Andrew J., et al. "Estimation of retinal ganglion cell loss in glaucomatous eyes with a relative afferent pupillary defect." Investigative Ophthalmology & Visual Science 55.1 (2014): 513-522.
Unilateral periodic pupillary constriction causing alternating anisocoria
Conrad, Erin C., et al. "Unilateral periodic pupillary constriction causing alternating anisocoria." Neurology 90.2 (2018): 86-88.
Detecting glaucoma using automated pupillography
Tatham, Andrew J., et al. "Detecting glaucoma using automated pupillography." Ophthalmology 121.6 (2014): 1185-1193.
Detecting Glaucoma with Pupillography
Chang, Dolly S., et al. "Detecting Glaucoma with Pupillography." Investigative Ophthalmology & Visual Science 53.14 (2012): 5621-5621.
Pupillographic evaluation of relative afferent pupillary defect in glaucoma patients
Ozeki, Naoki, et al. "Pupillographic evaluation of relative afferent pupillary defect in glaucoma patients." British Journal of Ophthalmology 97.12 (2013): 1538-1542.
Does the American Academy of Ophthalmology and the American Optometric Association recommend pupillary testing for POAG glaucoma suspects and patients?
Is there a CPT Code for quantitative pupillometry (USA Customers only)
Quantitative pupillometry with physician or other qualified health care professional interpretation and report, unilateral or bilateral.
Is pupillary light reflex testing (using the swinging flashlight method or EyeKinetix) a required element of a comprehensive eye exam?
How long does the pupillary light reflex test (RAPDx / APD protocol) take?
Are the APD results easy to interpret?
Does the absence of an APD mean there is nothing wrong with my patient?
How long is the scotopic / photopic pupil measurement (Low-High protocol)?
Does EyeKinetix qualify for the ADA tax credit? (USA Customers only)
Testimonials

“Coincidence you contacted me today, as this same day I detected new open angle glaucoma in a 28 year lady in for regular eye exam. She has 20/20 vision without glasses and has an exam once every 5 years. Without my RAPDx® this glaucoma could have easily slipped by and she would suffer 5 more years of retinal nerve damage.
The RAPDx®/EyeKinetix® is truly amazing technology. It has saved the sight of numerous patients and build my glaucoma practice along the way.
Thank you to Konan for transforming eye disease detection and patient care!”
Glen R. Owen, OD, FAAO

The RAPDx® score provides a highly sensitive and specific assessment of the RAPD compared to the swinging flashlight method. It is easily used by ancillary personnel as part of the screening of patients and is a powerful tool for clinicians needing to identify, confirm and quantify relative afferent pupillary defects.”
Nicholas J. Volpe, MD

“I have diagnosed over a dozen patients with low-tension glaucoma with RAPDx®. These patients had a relative afferent pupillary defect as their initial abnormal finding and without the benefit of automated objective pupillography, my index-of-suspicion for ocular disease would have been lower and I might have missed the diagnosis.”
Craig Thomas, OD

“RAPDx® is beneficial in my practice to easily and precisely quantify afferent pupillary abnormalities as well as accurate and quantitative documentation of follow-up progress in patients with diseases of the anterior visual pathways. In addition, RAPDx® helps me detect subtle RAPDs in the early diagnosis of diseases, such as glaucoma, and to document the absence of an RAPD in non-organic, unilateral, vision loss.”
Swaraj Bose, MD

“The EyeKinetix® provides peace of mind that our patient’s pupillary reflexes are being evaluated accurately and objectively. I have found the unit to be so much faster than its predecessor, RAPDx®, and much more user/operator friendly. With the speed of EyeKinetix® we do not have a bottle neck at our testing stations – it allows us to maintain the preliminary testing production flow. This instrument is going to help us save someone’s life, or quality of life, by picking up subtle APD producing pathology—that we probably were going to miss. I believe in the unit so much that I have ordered 2 of them for our office.”
Mario Gutierrez, OD, FAAO

The biggest problem with RAPD testing is that eyecare providers don’t do it … I estimate that pupillary testing is documented only about 10% of the time. It used to be gonioscopy took the prize for being done seldom and badly …”


